Is 2019 the Year of the Patient Voice?
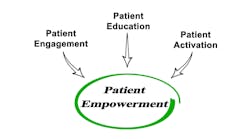
The 10th Health Datapalooza conference is coming up March 27-28, and its unofficial motto has always been “Nothing About Me Without Me.” That focus on participatory healthcare finally seems to be gaining traction in health systems as provider groups make the connection between recording patients’ preferences and impressions and improved outcomes.
Sometimes journalists write a series of stories and only after they are written do they realize a common thread. That is what happened to me the other day when I was listening to Lisa Schilling, R.N., M.P.H., vice president of quality, safety and clinical effectiveness at Stanford Health Care in California, speak about improving patient safety in the ambulatory setting. Referring to care coordination and transitions of care, Schilling said, “If you don’t use patient engagement methods like OpenNotes and co-design of your interventions with patients, teach back, and shared decision-making, now is the time to do that.”
That reminded me of a story I wrote last week about the deployment of a platform called PatientWisdom being rolled out at the regional network of Froedtert Health and the Medical College of Wisconsin. Describing their efforts to humanize the electronic health record, Jeana Holt, D.N.P., R.N., a primary care postdoctoral research fellow in the Department of Family and Community Medicine at the Medical College of Wisconsin, said, “We ask patients to provide things about their life: their joys, their challenges, their preferences and their values regarding their care.” In patient focus groups, she adds, they have been very supportive and say this is the first time they have been asked these types of questions. “It causes them to positively reflect on what their goals and values are regarding their health.”
Yale New Haven Health has expanded its use of the PatientWisdom solution across the continuum of inpatient and outpatient care, including the Yale Medicine practices, and Allina Health in Minnesota just announced a new partnership with PatientWisdom Inc.
There is also a movement under way to introduce electronic patient-reported outcomes (ePROs) into the routine practice of oncology providers to improve symptom management and to decrease hospitalizations.
Late last year I wrote that the National Cancer Institute, in association with the Beau Biden Cancer Moonshot Initiative, is funding the collaboration, the SIMPRO (Symptom Management IMplementation of Patient Reported Outcomes in Oncology) Research Center. The SIMPRO team is working with Epic, the EHR system used by all six participating institutions, which are New Hampshire-based Dartmouth-Hitchcock, Dana-Farber/Brigham and Women’s Cancer Center in Boston, Baptist Memorial Medical Center in Memphis, Lifespan Cancer Institute in Rhode Island, West Virginia University Cancer Institute, and Maine Medical Center in Portland.
Researchers also are studying the impact of adding patient narrative in clinical trials. A recent study by the University of North Carolina Lineberger Comprehensive Cancer Center found that allowing patients to write, in their own words, about treatment-related symptoms they experienced while participating in clinical trials can provide valuable information.
Their study, published in the Journal of the American Medical Informatics Association, examined two different methods of collecting symptom information directly from patients during clinical trials: They could either write in their own symptoms or choose them from a library of medical terms. When patients chose to write about their own symptoms in the study, a wide range of additional issues were revealed, ranging from pain and insomnia to muscle spasms, mouth sores and challenges with concentration.
“Currently, the standard practice for trying to capture symptom information directly from patients involves using trial-specific questionnaires,” said the study’s lead author UNC Lineberger’s Arlene Chung, M.D., assistant professor of medicine and pediatrics, and associate director of health and clinical informatics in the UNC School of Medicine, in a prepared statement. “Our research reveals that this approach may not be sufficient to capture what patients are experiencing during cancer treatments, and offering a free-text functionality provides important information about additional symptoms.”
Researchers continue to study the impact of OpenNotes. In a recent study in Applied Clinical Informatics, the majority of patients surveyed (83%) thought OpenNotes helped them take better care of themselves, without increasing worry (94%) or contacting the physician after reading the note (91%).
Getting back to the upcoming Health Datapalooza, I noticed that one of the panel sessions is titled “Nothing about Us without Us: Toward Collective Self-Governance of Patient Support Groups' Data on Social Media.” Here is the description: “A massive security vulnerability was discovered which allowed PHI to be leaked from closed support groups on Facebook. In this session we’ll discuss how a coalition of patients and security researchers faced this crisis and explore the need to develop a new model for collective data governance on social media.”
It's good to see the conference staying true to its roots in the patient data access movement. And I will keep looking for other examples of innovations that bring the patient’s voice to the forefront of care.