Leaders Are Advancing the Patient Experience—Across Diverse Environments
It really was fabulous to sit down with a panel of health system leaders who are leading the entire healthcare system forward around patient engagement and the patient experience, on Thursday morning, in Los Angeles, during our Healthcare Innovation California Summit, held last week Wednesday and Thursday, November 2 and 3, at the Sofitel Hotel Los Angeles at Beverly Hills.
Under the heading, “Patient Engagement: Revisioning the Patient Experience,” I was joined by Anshu Abhat, M.D., M.P.H., director of patient engagement in Office of Patient Access, in the Department of Health Services, Los Angeles County, and also a practicing primary care physician at Harbor-UCLA Medical Center; Margeaux Akazawa, M.P.H., manager of digital transformation at Children’s Hospital Los Angeles; Alan Dubovsky, vice president and chief patient experience officer at Cedars-Sinai Health; and Carrie Kozlowski, O.T., co-founder and chief operating officer at the Chicago-based Upfront Healthcare.
Every one of the panelists is an expert in her or his own right; but together, they offered our audience an amazing cornucopia of insights into the healthcare system-wide journey that our entire U.S. healthcare system is facing. Among other things, we discussed how the pandemic has both opened the eyes of everyone inside healthcare to some of the really challenging gaps in process that can improve the patient and family experience, while at the same time, opened the eyes of patients and families, as the consumers of healthcare, to their potential power to change the dynamics around their lived experiences inside the healthcare system.
Of course, each panelist shared about somewhat different dynamics and landscapes around the patient experience. Dr. Abhat noted that nearly all patients cared for at Harbor-UCLA are on MediCal (what Medicaid is called in California) or are uninsured, so, by definition, they are marginalized individuals, whose social-determinant needs are high. The population cared for at her medical center and whose overall care the Department of Health Services for Los Angeles County monitors, is also incredibly diverse, with many of the individuals and families not speaking English as a first language, or fluently. The same is true at Children’s Hospital Los Angeles, Akazawa confirmed, with a majority of individuals and families having a first language other than English. By definition, that requires clinicians and others in the organization to think very strategically about how to meet patients and families where they are, and to meet their needs broadly, beyond purely clinical concerns.
Meanwhile, as Dubovsky noted, Cedars-Sinai is famous in the media and public consciousness as “The Hospital to the Stars”; but, he emphasized, the vast, vast, vast majority of Cedars patients are just regular people; and that organization’s patients and families are also extremely diverse. One thing that he and his colleagues have been doing has been to consistently leverage data analytics to help them figure out exactly what’s going on, and how they can improve the patient experience. Akazawa and her team are also moving forward with analytics in their sphere. And Kozlowski’s entire company is focused on leveraging analytics to help patient care organization leaders figure out where the true gaps and issues are, and to marry analytics work with the continuous improvement of the dynamics that patients and families experience in all their encounters with the healthcare system.
All of these panelists are leading teams that are helping to show the way forward in this incredibly important area. And, as I referenced on the panel, the patient engagement/patient experience area is one in which innovation is exploding, in the best way possible. On the one hand, there is no simple playbook or template to follow in this area; but it’s also one in which the leaders of patient care organizations nationwide are demonstrating striking innovation, creating all sorts of new innovations that are responding to the needs of the patients and families they’re caring for.
And this has all been validated by the survey that we executed this spring, and reported on in our Patient Engagement Executive Handbook. Among other things, we found that:
Ø Fully 41.4 percent report that their organizations are “already active and moving forward with our integrated patient engagement/patient experience strategy”
Ø Another 40.77 are actively developing a strategy, though are in the early stages of their
Ø Only 17.83 percent have not begun any work at all in this area
Not only were those results heartening with regard to the overall forward evolution of work around the patient experience; that survey was conducted earlier this year, and it’s clear from all of our reporting and research since then that progress is accelerating rapidly now in patient care organizations across the country. The evidence of all this is everywhere; and of course, some organizations have actually been at it for a while now. For example, Aaron Martin, who was executive vice president chief digital officer of the 52-hospital, 1,085-clinic, Seattle-based Providence Health & Services, but who recently went back to Amazon, where he had been an executive before joining Providence, told us this spring that “Providence has been focused on this for eight years now. We’ve been primarily focused on improving the digital experience, with the rationale involving a few elements. One is that it’s a lot easier to change or iterate a digital-first experience that’s compelling, than to launch new physical clinics, etc. We’ve also separately been making changes in the in-clinic experience, in terms of how we present ourselves to patients.” Among the issues that the Providence leaders have been working on are improving access, making pricing more transparent, and improving patient and family navigation between and among care sites.
What’s more, reacting to the survey result that found that 17.83 percent of respondents said their organizations have not yet begun any work in this area, Randy Gaboriault, chief digital and information officer at the three-hospital ChristianaCare health system in Wilmington, Delaware, told us that “The 18 percent organizations will not be the longest-running organizations in America. So, flat out, in the world we’re living in, experience has to become the organizing principle; it’s that clear. And if you haven’t even begun to pursue a strategy, I’m not sure that you’ve ever shopped or banked virtually. There’s clear spillover into healthcare from other areas of our lives. And there are disruptors that begin with experience as their thesis,” he added.
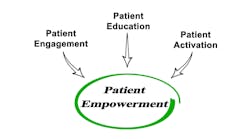
And, of course, when the leaders of patient care organizations reference the concepts of patient engagement and the patient experience, individuals may in fact have different conceptual and practical reference points in their minds. As Terri Hanlon-Bremer, R.N., M.S.N., told us this spring, “It's a great first question. A couple of things: one, I’m always curious about how they define patient experience.” Hanlon-Bremer is senior vice president of employer solutions and population health at the Cincinnati-based TriHealth, a two-hospital, 130-site-of-care integrated system in southwestern Ohio. “We’ve been measured by HCAHPS scores, for years,” she told us, referencing Medicare’s Hospital Consumer Assessment of Healthcare Providers and Systems Survey. “And those measures were seen as measuring the patient experience. So in that sense, no, since we’re graded on that. What I think would be a more interesting question is, how does a healthcare organization define a patient experience? We’ve looked at it through a traditional lens, but now, we’ve shifted to more of a consumerism mentality. I don’t think there are a lot of organizations yet truly focused on the consumer’s journey.”
Importantly, because of learnings coming out of the intense COVID-19 pandemic months, leaders in patient care organizations nationwide are figuring out how to strategize and forge ahead despite challenging internal headwinds. As what the biggest barriers are to implementing programs around patient engagement and the patient experience, survey respondents this spring cited “goals and objectives competing for our time and attention” (66.95 percent); “lack of both financial and human resources” (29.66 percent); “lack of strategic direction/consensus” (22.88 percent); “lack of human resources” (16.95 percent); “lack of financial resources” (11.86 percent); “lack of support from the c-suite” (9.32 percent); and “lack of support from the board” (0.85 percent). Yet, from the evidence of the discussion last week in Los Angeles, organizational leaders are simply forging ahead, despite the challenges facing them. Certainly, hearing from Anshu Abhat and Margeaux Akazawa about how assertively their teams are moving forward—even as both organizations are perpetually resource-constrained—says to me that a head of steam is building healthcare system-wide around all these initiatives.
Everyone will agree that 2022 has been a challenging year in healthcare, for a host of reasons. But the progress being made in the patient engagement/patient experience arena speaks to me of great hope and great enthusiasm among key leaders in patient care organizations nationwide. Let a thousand flowers blossom!